APS can be found as a lone diagnosis but may occur concomitantly with other autoimmune diseases.
Introduction
Antiphospholipid syndrome (APS) is an acquired systemic autoimmune disease where the body’s immune system produces antibodies that affect phospholipids. APS is found in approximately 15-20% of women with RPL, representing the most frequently identifiable risk factor amenable to treatment.1, 2
APS can be found as a lone diagnosis but may occur concomitantly with other autoimmune diseases. For example, patients with APS may also have a diagnosis of Systemic Lupus Erythematosus (SLE).
APS presents with a range of clinical phenotypes, including poor reproductive outcomes (recurrent pregnancy loss, preeclampsia, preterm birth, fetal growth restriction and stillbirth), venous and arterial thrombosis, and rash.
Investigations
- Women with RPL should be tested for APS by obtaining blood and testing for lupus anticoagulant (LA) and anti-cardiolipin (aCL) (IgM and IgG) antibodies.
- A long time between venesection and laboratory processing can quench the lupus anticoagulant and yield a false negative result.
- The diagnosis is made with the detection of LA or aCL on two separate occasions, 12 weeks apart.1
- Anti-beta-2-glycoprotein1 (β2GP1) may be measured to aid diagnosis.3
- Repeat testing is only recommended if an initial APS antibody test is positive or indeterminate.
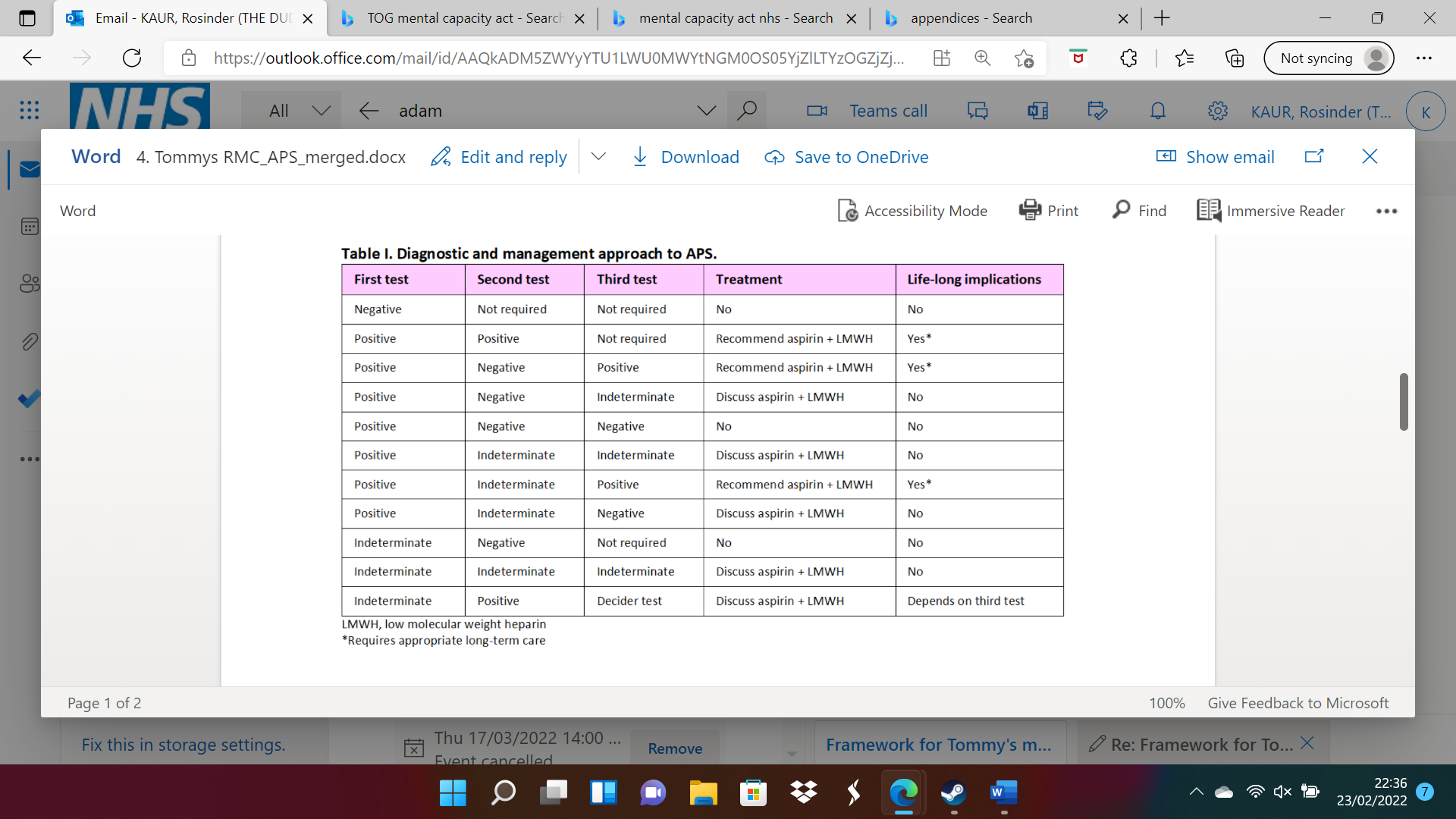
- Some women require a third ‘decider’ test (Table 1).
- Testing should be postponed 6 weeks following a pregnancy (loss).
- Positive women should have a full blood count to assess for thrombocytopaenia.
- Women with APS should receive specialist pre-conception counselling and joint obstetric-haematology ‘high-risk’ care.
- The general practitioner (GP) should be informed due to the long-term increased risk of arterial and vascular disease.
- Patient education regarding treatment adherence and lifestyle counselling, including smoking cessation and body mass index, is important.
Table I. Diagnostic and management approach to APS.
Treatment
- Women with APS should receive:
o Aspirin 75 mg once daily from the time of a positive pregnancy test AND
o Low molecular weight heparin (LMWH) at a weight-adjusted prophylactic dose from confirmation of an intrauterine pregnancy on ultrasound scan, to be continued for six weeks postnatally. For example:
- <50 kg: enoxaparin 20 mg once daily
- 50-90 kg: enoxaparin 40 mg once daily
- 91-130 kg: enoxaparin 60 mg once daily.4
o The dose of aspirin should be reviewed at the woman’s booking appointment and increased to 150 mg once daily for the prevention of preeclampsia where applicable.
- Local obstetric policy should be observed if different from RCOG guidance.
- Women who take LMWH do not need to have platelet count monitoring for heparin-induced thrombocytopaenia, but should be informed of the adverse events associated with this drug as below.
- Contraindications to aspirin: known peptic ulceration, bleeding disorders, haemophilia, severe cardiac failure.
o Use aspirin with caution in women with anaemia, asthma, G6PD deficiency, hypertension, thyrotoxicosis.
o Aspirin and LMWH should be discontinued if there is acute bleeding in pregnancy, and women should be advised to contact their RPL clinic.5
- Contraindications to LMWH: increased bleeding tendency and thrombocytopaenia. In these circumstances, referral to a haematologist should be made. LMWH should be discontinued if there is acute bleeding in pregnancy, and women should be advised to contact their RPL clinic.
- Women with APS should be informed that combined aspirin and LMWH therapy is superior to aspirin alone to reduce their risk of miscarriage and increase live birth rates.
- Combined aspirin and LMWH should be discussed with women with borderline APS test results (Table 1), although the benefit of treatment is less certain.
- Women with a history of thrombosis may require increased doses of LMWH as directed by a haematologist.
- The woman should be advised to inform her community midwife at the time of booking that she is taking aspirin and LMWH so that onward appropriate antenatal clinic referral can be made.
Specialised and long-term care
- Women with APS have a long-term increased risk of arterial and vascular disease.
- Women with APS should receive specialist pre-conception counselling and joint obstetric- haematology ‘high-risk’ care due to an increased risk of thrombotic and obstetric complications.
- The GP should be informed due to the long-term increased risk of arterial and vascular disease.
- Patient education regarding treatment adherence and lifestyle counselling, including smoking cessation and body mass index is important.
References
- Bender Atik R, Christiansen OB, Elson J, et al. ESHRE guideline: recurrent pregnancy loss. Human Reproduction Open 2018. DOI: 10.1093/hropen/hoy004.
- Quenby S, Gallos ID, Dhillon-Smith RK, et al. Miscarriage matters: the epidemiological, physical, psychological, and economic costs of early pregnancy loss. Lancet 2021;397:1658-1667. DOI: 10.1016/s0140-6736(21)00682-6.
- Definitions of infertility and recurrent pregnancy loss: a committee opinion. Fertility and Sterility 2013;99:63. DOI: https://doi.org/10.1016/j.fertnstert.2012.09.023.
- RCOG. Reducing the Risk of Venous Thromboembolism during Pregnancy and the Puerperium: Green-top Guideline No. 37a. April 2015.
- BNF 81 : March-September 2021. London: British Medical Association, 2021
Leave A Comment